Mohs Skin Cancer Surgery
The following information has been taken from the pamphlet, “Important Patient Information Regarding Mohs Micrographic Surgery in the Treatment of Skin Cancer”, provided by the American Society for Mohs Surgery.
What is Mohs Micrographic Surgery?
Mohs micrographic surgery is a specialized, highly effective technique for the removal of skin cancer. The procedure was developed in the 1930s by Dr. Frederic Mohs at the University of Wisconsin and is now practiced throughout the world. Mohs surgery differs from other skin cancer treatments in that it permits the immediate and complete microscopic examination of the removed cancerous tissue, so that all “roots” and extensions of the cancer can be eliminated. Due to the methodical manner in which tissue is removed and examined, Mohs surgery has been recognized as the skin cancer treatment with the highest reported cure rate.
The Mohs Surgical Procedure
Typically, Mohs surgery is performed as an outpatient procedure in the physician’s office. Although the patient is awake during the entire procedure, discomfort is usually minimal and no greater than it would be for more routine skin cancer surgeries. The Mohs surgical procedure is illustrated in the following diagrams:
Stage 1
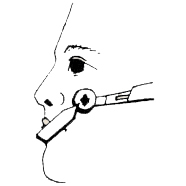
Figure A
The area to be treated is cleansed, marked, and injected with a local anesthetic. The Mohs surgeon removes the visible cancer, along with a thin layer of additional tissue (Stage 1). This procedure takes only a few minutes, and the patient waits while tissue is being processed and examined.
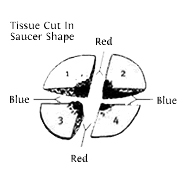
Figure B
The removed tissue specimen is cut into sections, stained, and marked on a detailed diagram (Mohs map).
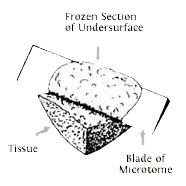
Figure C
Tissue is frozen on a cryostat, and technician removes very thin slices from the entire edge and undersurface. These slices are then placed on slides and stained for examination under the microscope. (This is the most time-consuming portion of the procedure, often requiring one hour or more to complete.)
Stage 2
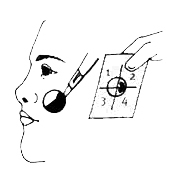
Figure D
The Mohs surgeon carefully examines the entire undersurface and complete edge of the specimen, and all microscopic “roots” of the cancer are precisely identified and pinpointed on the Mohs map. Upon microscopic examination, if residual cancer is found, the Mohs surgeon utilizes the Mohs map to direct the removal of additional tissue (Stage II). Note that additional tissue is removed only where cancer is present.
Stage 3
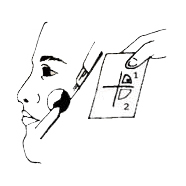
Figure E
This process is repeated as many times as necessary to locate any remaining cancerous areas within the tissue specimen (Stage III, Stage IV, etc.)
Stage 4
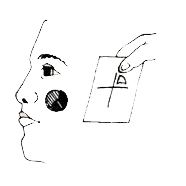
Figure F
When microscopic examination reveals that there is no remaining tumor, the surgical defect is ready for repair.
Free Consultation
Moh’s Surgery FAQ’s
Special Qualifications of the Mohs Surgeon
Physicians performing Mohs surgery should have specialized skills in dermatology, dermatologic surgery, dermatopathology, and Mohs surgery. Basic and advanced training in Mohs surgery is available through selected Residency programs, specialized fellowships, observational preceptorships, and intensive training courses. In addition, the Mohs surgeon must have the required surgical and laboratory facilities and must be supported by a well-trained Mohs nursing and histotechnological staff. Your Mohs surgeon can provide you with detailed information regarding his or her training in the above disciplines, as well as all applicable professional affiliations. To learn more about the American Society for Mohs Surgery, please refer to the back page of this brochure.
Advantages of the Mohs Surgical Procedure
Some skin cancers can be deceptively large – far more extensive under the skin than they appear to be from the surface. These cancers may have “roots” in the skin, or along blood vessels, nerves, or cartilage. Skin cancers that have recurred following previous treatment may send out extensions deep under the scar tissue that has formed at the site. Mohs surgery is specifically designed to remove these cancers by tracking and removing these cancerous “roots.” For this reason, prior to Mohs surgery it is impossible to predict precisely how much skin will have to be removed. The final surgical defect could be only slightly larger than the initial skin cancer, but occasionally the removal of the deep “roots” of a skin cancer results in a sizable defect. The patient should bear in mind, however, that Mohs surgery removes only the cancerous tissue, while the normal tissue is spared.
Special Indications for Mohs Surgery
This consultation session provides advice for the daily skin care routine, emphasizing aspects of healthy skin maintenance, prevention and correction of aging and sun damage. We introduce our patients to professional, cutting edge skin care products as part of a multifactorial approach to enhance skin appearance and texture. You will also have the opportunity to be educated on each procedure offered in our office.
Insurance Coverage for Mohs Surgery
Most insurance policies cover the costs of Mohs surgery and the reconstruction of the resultant surgical area. Please contact your insurance carrier directly for the most current payment information relative to this surgery. The insurance billing department in your Mohs surgeon’s office also may be able to assist you.
Patient Preparation for Surgery
If you are taking prescription medications, continue to take these unless otherwise directed by a physician. However, you should inform your Mohs surgeon if you are taking blood-thinning medications such as coumadin, Plavix, aspirin, aspirin substitutes (such as Advil, Motrin, Nafton, Naprosyn, etc.), vitamin E, gingko, garlic, ginseng, ginger, ephedra or other nutritional supplements. These medications and supplements can sometimes cause an increased chance of bleeding after surgery.
It is important that you obtain a good night’s rest and eat normally on the day of your surgery. For your comfort, it is recommended that you wear casual, layered clothing. You may also wish to bring a light snack and a book or magazine to help occupy your waiting time. Also, it may be advisable to arrange for someone to drive you home following surgery, if needed.
Duration of Procedure
Most Mohs cases can be completed in three or fewer stages, requiring less than four hours. However, it is not possible to predict how extensive a cancer will be, as the extent of a skin cancer’s “roots” cannot be estimated in advance. Therefore, it is advisable to reserve the entire day for this surgical procedure, in case the removal of additional layers is required.
Minor Post-Surgical Discomfort Expected
Most patients do not complain of significant pain. If there is some discomfort, normally only Tylenol is required for relief. However, stronger pain medications are available and will be prescribed when needed. You may experience some bruising and swelling around the wound, especially if surgery is performed near the eye area.
Options for Post-Surgical Reconstruction
After the skin cancer has been removed, your Mohs surgeon will discuss the following options with you:
- Allowing the wound to heal naturally, without the necessity of additional surgery (which may produce the best cosmetic result).
- Simple or complex wound repair performed by the Mohs surgeon.
- Referral to the original referring physician for wound repair.
- Referral to another surgeon for wound repair.
If your wound requires daily care at home, you will be given detailed instructions following your surgery. For small post-surgical sites, direct closure by suturing the sides of the wound together may be possible. However, in certain areas of the body, there is very little tissue that can be stretched for coverage of a wound, and either a skin graft or skin flap must be used. In closing wounds with a skin flap, the skin adjacent to the surgical defect is partially cut free, and then rotated or moved forward to cover the surgical area. Stitches are then placed to hold the flap in its new position. This provides immediate coverage for the wound. Other areas may require a skin graft to provide coverage. Skin from the side of the neck, behind the ear, or over the collarbone may be cut free, placed over the wound, and then sewn into place. The original site of the graft is then closed with stitches or allowed to heal on its own.
Wound Healing, Scarring, and Scar Revision
As with all forms of surgery, a scar will remain after the skin cancer is removed and the surgical area has completely healed. Mohs micro-graphic surgery, however, will leave one of the smallest possible surgical defects and resultant scars. Often, wounds allowed to heal on their own result in scars that are barely noticeable. Even following extensive surgery, results are frequently quite acceptable. In addition, scars do have the ability, through the body’s own natural healing properties, to remodel and improve in appearance for a six to twelve month period. There are also many other techniques available to the patient for enhancement of the surgical area following skin cancer surgery. Depressed or indented scars may be elevated, using an implant such as Zyderm collagen. Likewise, a raised or roughened scar may be smoothed, using laser resurfacing or chemical peeling techniques. Skin flaps and grafts also may require a subsequent “touch up” procedure, to further improve their appearance.
Potential Complications Associated With Mohs Surgery
Patients should understand that there is not an absolute guarantee that any given procedure will be totally free of complications or adverse reactions. Mohs surgery is no exception. During surgery, tiny nerve endings are cut, which may produce a temporary or permanent numbness in and around the surgical area. If a large tumor is removed or extensive surgery is required, occasionally a nerve to muscles may be cut, resulting in temporary or permanent weakness in a portion of the face. This is, however, an unusual complication. The surgical area may remain tender for several weeks or months after surgery, especially if large amounts of tissue were removed. Rarely, some patients experience intermittent itching or shooting pain in the surgical area. In addition, the skin grafts and flaps used to cover surgical areas may not fully survive, requiring additional repair.
About the American Society for Mohs Surgery
The American Society for Mohs Surgery was established in 1990, and has experienced continued growth while honoring its commitment to the organization’s original tenets:
“The purpose of this organization shall be to promote the highest standards of patient care relating to Mohs surgery for the surgical removal of skin cancer and other appropriate malignancies; to establish quality assurance and regular peer review of Mohs surgeons; to provide a forum for the exchange of ideas and methodology for Mohs surgery and related basic sciences; to promote the professional education of its members and the medical community in the principles and practice of Mohs surgery; to encourage research into all methods of microscopically controlled removal of malignant tissue; and to provide information for public education relating to Mohs surgery.”
For additional information regarding the American Society for Mohs Surgery, its membership qualifications, and educational programs, please contact our administrative office or visit our Web site.